|
| Kenneth Brein, M.D. |
He did well at Harriton High in Lower Merion just outside of Philadelphia, and he thought he’d be a scientist. His father (who, said Ken, joined the Army after graduating from Overbrook High but then struggled in a variety of businesses) recognized his third son’s potential. His often-whispered advice to Ken? “Be a doctor, be a doctor...”
But when Ken finished high school in 1974 near the top of his class of 250 his plan was to study science and engineering, not medicine. He applied to four elite schools and when he visited Princeton’s 500-acre bucolic campus it was “a gorgeous day in April.” When he toured Penn in West Philadelphia, it was a gloomy rainy day. So, Princeton it would be.
 |
| Princeton University in the spring (from the Fulbright Commission) |
While in central New Jersey, Ken refined his interests and decided to study biomedical engineering. But the course offerings were limited. He took whatever he could, and for his senior thesis he wrote the complex math for a theoretical model of blood flow (a fluid, but with cells floating in it) through the small tubes of an artificial lung. Ken was (once again) advised to go to medical school.
So he applied to a number of medical programs, received acceptances, and chose Penn (despite his weak first impression of the area). He enjoyed learning biology and doing medicine but seemed to lose interest in research. And as he progressed through the various rotations, he didn’t develop a feeling for a particular specialty. But one day, he was given a nudge. This happened when he was visiting his mother and her second husband George at their apartment on leafy Rittenhouse Square in downtown Philadelphia.
WHY OPHTHALMOLOGY
 |
| Dr. Zubrow |
Ken thought for a bit. Maybe he’d go into Hematology-Oncology, he said, having recently done an intense rotation in that.
“Try something else,” said Dr. Zubrow flatly.
“Maybe Cardiology?” (Surely, Dr. Zubrow would be happy with that answer, thought Ken.)
“Try something else,” was the cryptic response.
“Maybe Infectious Disease?”
“Try something else,” came the reply once more.
By that point, the perceptive medical student began to catch on.
“Oh. Well…ophthalmology looks pretty good,” offered Ken.
“That’s a good one,” said Dr. Zubrow.
“Maybe Dermatology?“ Ken guessed as he was guided along.
“That’s a good one.”
The attentive pupil was “getting the message, loud and clear.” And when the time came to decide on the next phase of his training, a residency, Ken chose to study the many diseases of the eye. He would have loved to have gone to the Will's Eye in Philly but was content to be accepted into the ophthalmology program at the University of Pittsburgh. So, after medical school, and a year of internship at Pennsylvania Hospital (where a portrait of Dr. Zubrow is prominently displayed) he and Jessica took the turnpike (called “America’s First Superhighway” when it opened in 1940) 300 miles west. Wait a minute! Did I forget something? Who’s this Jessica?
 |
| UPMC Presbyterian Complex in Pittsburgh (from UPMC) |
Well, during the Christmas break the first year of medical school Ken took the train to Manhattan to visit one of his college roommates. When it was time to head back to Philadelphia he boarded at the busy Penn Station. He realized that he forgot to bring a book or a newspaper to keep him occupied for the hour-plus trip. What was he going to do? As he made his way down the aisle of the crowded car he spotted an empty seat next to a pretty girl. Somehow, he had the intuition that she was from Long Island and returning to Penn (no, she was not wearing the U of P red and blue). He thought they might hit it off.
So he sat down next to her, but she made an expression like ”you're invading my space.” He would have to play his cards right. So Ken, trying to be optimistic and trying to impress, reeled off his credentials (you see, he didn’t have a guitar with him). After chatting for a while, he asked her to dinner. But Amy (that was her name) was on her way to Penn to see her (quick stab in the heart) boyfriend. However, “I have a sister you might like,” she said. So she gave Ken Jessica’s phone number. What did he have to lose? He decided to give her a cautious call and soon wined and dined her, taking her to the fancy “La Terrasse” French bistro on the Penn campus. I guess it worked out, as they married and have three adult children and six grandchildren.
 |
| Watercolor of the well-known Locust Walk at Penn (by elliemoniz.com) |
AFTER RESIDENCY, WHERE TO PRACTICE?
Though Jessica would have been happy to stay in Pittsburgh after Ken finished his three-year residency, and he was offered an opportunity there, he wanted to be closer to the Jersey shore, to tiny Ventnor City, a two-square-mile vacation spot of many soothing childhood memories. So as Ken searched for a place to practice through print ads in the journals, he learned that Dr. Charles Letocha (also a product of Princeton and Penn) in York was looking for a partner. After a series of letters (yes, actual handwritten letters) back and forth, careful Chuck finally decided to meet Ken (and Jessica). They clicked right away, and Ken moved to York and joined the private practice in 1986.
As a clinical ophthalmologist, Dr. Brein focused his energies on perfecting his skill in cataract surgery, addressing the clouding of the lens in the eye that is the cause of half of the world’s blindness. But a type of blindness that can almost always be cured.
CATARACTS
Let’s talk about the cataract. The clear crystalline lens focuses incoming light to the fovea at the back of the eye, the area of the retina with the highest density of light-sensitive cones serving color vision. With age, (and UV light exposure) the proteins in the lens change and coalesce and the lens becomes progressively opacified, letting less and less light pass through. Though attempts to stick a sharp needle into the eye (ouch!) to push the clouded lens out of way go back as far as the fifth century BCE in India, the first “modern” cataract surgery was performed by a French surgeon in 1747. Serious complications were not unusual, and vision after the procedure was poor; thick heavy “Coke bottle” glasses were needed to see clearly in the absence of a lens.
So physicians used to wait until there was a nearly complete loss of vision before removing the severely opaque lens. But advances in surgical techniques eventually made the procedure much safer. And Dr. Brein said that cataract surgery was revolutionized by Dr. Charles Kelman in 1967. He devised a procedure termed phacoemulsification. With this, a thin ultrasound-driven needle inserted through a tiny incision breaks up then and then sucks it out. This is a very safe technique. It is the standard now, though it took a while to catch on (like most bold innovations in medicine).
The development of the plastic artificial lens in 1974 by Dr. Harold Ridley in London to replace the worn-out body part provided a much more satisfying vision outcome for patients. And when the foldable plastic lens was invented in 1980, the incision required to insert it became even smaller and less traumatic.
 |
| Phacoemulsification and intraocular lens implant (artwork by Christine Cote) |
For experienced surgeons, like Dr. Brein and his partners, cataract surgery became extremely controlled and consistent. And it is claimed that nearly 98% of patients can expect a successful outcome, a truly remarkable statistic for any surgical procedure. Complex lenses can now correct a variety of refractive errors, like astigmatism, etc. Over his satisfying 31 years in practice, Dr. Brein was able to deliver better sight to many thousands of individuals in York.
HE HAD TO STOP DOING SURGERY
But Dr. Brein had to stop performing the extremely delicate surgery after he developed nerve injuries affecting the strength and coordination of his right hand. He underwent surgery for median and ulnar entrapment, but recovery of dexterity was slow and he did not want to expose his patients to the risk of a slip-up (fear of such things during his practice would sometimes keep him up at night) so he put away his scalpel. He still saw patients for refractions and for the diagnosis of the many ailments that can affect the eye, but he could no longer offer them his surgical expertise. He was okay with that, but then something else happened.
ANOTHER BLOW
This next part of Ken’s story is particularly difficult to take in. And it was painful for me to hear. It happened five years ago.
It was a routine day at his office. For a few weeks, Ken had been experiencing what he thought was right-sided tooth pain spreading into his cheek. He did what many doctors do (and shouldn’t): he diagnosed himself. He assumed that he had developed maxillary sinusitis. But when Ken spoke with his wife from the office he sounded confused. It was clear to her that something serious was wrong. Jessica told him in no uncertain terms to stay put. That she was calling for emergency medical services. She then spoke with one of his partners, Dr. Matt Bilder, and said, “Make sure he gets into the ambulance.”
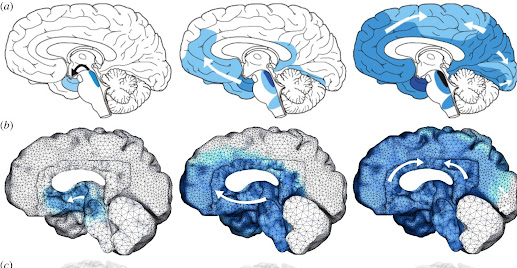
A head CT scan in the York Hospital ER showed that Ken had a right frontal lobe mass, an angry-looking mass compressing and distorting the brain. There was swelling and an ominous “midline shift.” He had to be admitted to the ICU to be monitored and watched closely. Later that night, he was wheeled away for an MRI.
Well, it turns out that Dr. Brein had created his Wellspan Health account a week before. With this part of the electronic health record, a patient can use their laptop or their phone to view their test results, any time of the day or night, wherever they are, even when they are in the hospital. So, lying in the ICU, with several IVs dripping and devices beeping and flashing and keeping time, alone in the darkness, he picked up his iPhone and cautiously opened his portal. There was a message: “You have a new test result.” The report of the MRI was already posted! Ken paused briefly, then opened the document. The radiologist felt that the mass was a tumor, “most likely a glioblastoma.” Ken, was very aware of the terribly grim statistics for survival after the diagnosis of a GBM and thought, “I’m dead.”
 |
| Images of a frontal GBM with a midline shift (from David C. Preston) |
“How were you able to deal with this?” I asked.
Ken waited for a moment, and then replied: “I have not said this before, but I think I went into denial.”
You see, when he was an intern in Center City Philadelphia he had taken care of a woman dying of this rapidly progressive untreatable tumor. So while he knew “intellectually” that he had received a death sentence he quickly determined that this harsh decree would not cripple him emotionally.
“Do you think you should have been allowed to view that MRI report, to be faced with such a grim diagnosis when you were alone?” I asked (but already knew the answer).
“No. I don’t think I should have been put in the position to see the test results at that point,” he answered. Sure, one of Ken’s doctors did come in the following morning to talk about his MRI and to explain things, but the psychic punch of facing imminent mortality had already landed; he said his “whole world was turned upside down” in that instant.
He recalled that early in the AIDS pandemic when there was no cure (there still isn't), and no effective treatment, the results of the testing for the HIV virus were to be given to the patient only with the help of a counselor. “That would have been helpful for me,” he said.
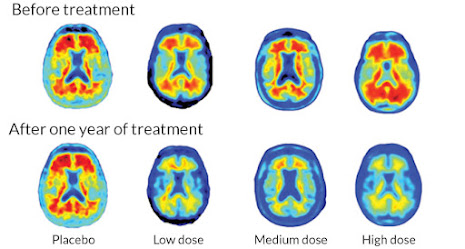
So, as a student of science and mathematics, Ken looked carefully at the dismal survival curves. While almost all patients died within two years (many in the first year), there was a tail of the curve to the right, an exceedingly small tail, but a tail nonetheless. In fact, it has been reported that about 5% of adults with a GBM survive five years and nearly 2% make it to ten years. He could, statistically, find himself in those tiny groups (higher physics and mathematics informed him that even exceedingly unlikely things do eventually happen).
 |
| GBM survival curves with different dosing of Temodar (from Bin Huang 2021) |
FOLLOWING THE DIAGNOSIS OF THE BRAIN TUMOR
After standard treatment with radiation and chemotherapy with Temodar, Ken’s oncologist in York found an ongoing trial of immunotherapy at Duke that appeared promising. Fortunately, Ken met the very strict criteria for the study. In that, they produced a personalized vaccine by harvesting some of his own white blood cells and exposing them to a specific antigen found in GBM tumors but not in normal brain tissue. They then injected these reactive cells into Ken’s thigh so they could find their way to the lymph nodes in his groin. Once there, they could generate T-cells to attack and destroy tumor cells carrying the targeted antigen. It seemed like a long shot, but it made sense to Ken to try; he had nothing to lose and everything to gain. (Two reported studies from Duke were very small, but 4 of 11 patients in one group and 2 of 6 in the other were alive at five years compared to 0 of 23 historical controls.)
Five years on, and after regular trips to Durham, and a bunch of noisy MRIs Dr. Brein, remarkably, has no evidence of recurrent disease. There is no talk of cure or even remission, he said, just no visible disease at this time. The “sword of Damocles” is still dangling precariously over his head, he noted.
WISDOM GLEANED“Have you changed over the past five years?” I asked (again, knowing the answer).
“ How can you not?” he replied.
Early on in his journey, he was given the simple advice to “make every day count.” At the end of each day, he and Jessica ask each other these few questions: Did we do something good today? Did we have fun today? So Ken tries to do what he enjoys. And he believes that his positive, attitude allows those around him to feel better, as well. For example, Ken has had the opportunity to meet with others coping with brain tumors like his. He discovered, somewhat to his surprise, that he could connect easily with them and that he could be compassionate in light of their shared experience. And he often imparts the wise counsel he received after his diagnosis. This has been rewarding. (Ken’s father, having lost a leg in an auto accident, helped console Veterans who had similar traumas.)
THE MUSIC
As Ken tries to follow his own guidance, (forced) retirement has had a “silver lining,” he said. It has allowed him to pursue his life-long interest in music in more depth. When Ken began playing the guitar he followed the popular rock and roll track. This served him well for many years. But when he, by chance, listened to a jazz album one day not too long ago he was struck by the colorful sound. There were different chords and chord progressions and complex harmonies. And there was an emotional element that intrigued him.
So he studied music theory; that there are specific patterns of sound frequency and rhythm that are especially pleasing to us, and moving. He studied the mathematics and the physics that result in, literally, “music to our ears.”
(My husband reminded me that there is no music or sound "out there," and no color. These are the private experiences the brain produces as it processes different wavelengths of energy detected by various sense organs. The tree that falls in the forest does not make a sound if is not perceived, it just disturbs the air. And he reminded me of Duke Ellington’s famous comment about music; "If it sounds good, it is good.")
Ken became serious about this and studied jazz guitar technique and theory (mostly online) with master guitarist and teacher Martin Taylor.
 |
| Music theory: The complicated (mathematical) circle of Fifths |
Ken is grateful to have been part of York’s “Unforgettable Big Band” for the past five years as they perform swing and classic big band music for appreciative audiences. He said that he has learned a lot from these talented and “professional musicians.” But he has been toying with the idea of playing solo jazz guitar in coffee house-type venues. And he might even try his hand at the intricate fingerwork of classical guitar.
AND MORE
Not content with sixteenth notes and syncopated rhythms and the physics of scales and harmonics, another one of Dr. Brein’s current interests is (wait for this…) cosmology, the study of the origin and development (and eventual running down) of the entire universe. Modern cosmology builds on insights about the curved fabric of space-time and elusive gravitational waves envisioned by Albert Einstein (a resident of Princeton in his later years). Remarkable insights that revolutionized our concepts about the nature of reality. (This, alone, should be enough to keep Ken plenty busy.)
And when he’s not with Jessica, or the rest of his family, or with his bands, or playing golf (where, he noted, you “keep your own score”), or fooling with one of his many guitars (including his first one), or reading stuff by Brian Greene or other cosmologists, you might find Dr. Kenneth Brein carefully covered up on the beach in Ventnor enjoying the peacefulness of the rolling ocean waves and the gently setting sun, the celestial fire sustaining life on Earth.
.jpg) |
| The quiet, soft, Ventnor City beach (from Shawn R. Smith) |
References and Suggested Readings:
1. MasterClass. "What is Jazz: A Guide to the History and Sound of Jazz." accessed at https://www.masterclass.com/articles/what-is-jazz (A succinct overview; but a start.)
2. Batich, Kristen, et. al. “Once, Twice, Three Times a Finding: Reproducibility of Dendritic Cell Vaccine Trials Targeting Cytomegalovirus in Glioblastoma." Clinical Cancer Research 2020 Oct 15;26(20):5297-530. (A report of the encouraging, though limited, experience at Duke, one of a number of centers looking for a way to shift the survival curve in GBM to the right.)
3. Greene, Brian. Until the End of Time: Mind, Matter, and Our Search for Meaning in an Evolving Universe. Alfred A. Knopf. New York, 2020. (Not just physics and math, but a far-ranging erudite exploration of what it means to be human and concluding that "in our quest to fathom the human condition, the only direction to look is inward." p. 326)
4. Davis, Geetha. "The Evolution of Cataract Surgery." Missouri Medicine 113(1): 58-62 2016.
By Anita Cherry 12/16/22