 |
| Dr. Lavallee |
They were looking for the “funny doughnuts,” buttery flaky French croissants. Mark recalled that Jacques, (host of popular TV documentaries in the late 1960s and early 70s on ocean life, and co-inventor of the modern SCUBA gear), was “super skinny and smelled like cigarettes.”
His Parents and Early Life
Mark’s father, Ray Lavallee, was from Northhampton, Massachusetts, before the family moved to Upstate New York just outside of Syracuse. He was an electrical engineer with GE and a defense contractor. Among other things, he developed and patented a sensitive microphone for so-called “Towed Array” sonar surveillance devices trailed behind ships. They allowed long-range detection and tracking of (quiet) Soviet nuclear submarines during the Cold War. |
| The restored 43-meter Calypso in 2016 (from the Cousteau Society) |
After Mom abandoned her Ph.D. aspirations she felt a calling to teach, but then gave that up temporarily to raise her three boys. One day, she took Mark to the pediatrician for an ear infection. The doctor had just read an article about a rare hereditary disorder of connective tissue called Ehlers-Danlos syndrome (EDS). The physician quickly recognized that Mark had this genetic condition of excessive joint mobility, soft stretchy skin, easy bruising, and poor wound healing with scarring. (Though it is much more than that, since the disorder may affect almost any organ.)
Anyway, a month after his fateful diagnosis, when Mark, the future Family Physician, Sports Medicine, and recognized EDS Specialist, was in the first grade, the family moved from the Syracuse suburb of DeWitt to the U.S. Naval base in Argentia in the Canadian Province of Newfoundland. Dr. Lavallee (the name is derived from the French “the valley”) told me that it was cold in the far north on the western edge of the Sea of Labrador and there were deep piles of snow for him and his brothers to play in (but it is not nearly as snowy as Syracuse, by the way).
 |
| A current view of Argentia, Newfoundland after the Naval base closed in 1994 (from Wikipedia) |
“Mrs. Lavallee, how are your children? And how many did God bless you with?” asked Mrs. Smith.
“I have three beautiful sons.”
“Uh, oh, problems in the bedroom Mrs. Lavallee?”
“No. Why do you say that?”
“Well this is Mrs. O’Conner, and she has been blessed with 21 children.”
“How many do you have?”
“I had 18, but lost two at sea.”
Small remote fishing communities, you see, often have large families for economic and cultural reasons. This allows them to survive and maintain their unique heritage and identity.
An Adventure/Misadventure
Well, after school was out for the year, his mother was “up for adventure.” She took her sons and one of their friends to “a park,” said Mark. She found a 1700s abandoned fort in “disarray.” Guys like that kind of stuff, right? It would be fun, right? But something awful happened.
The boys were running around, as they will do. Mark was exploring and creeping down a wooden stairway into “a basement or dungeon” (he wasn’t sure which) when the worn tread he stepped on gave way. His right leg fell through it. As a result of his fragile connective tissue the injury to his lower leg was devastating; from his knee to his foot, the skin and underlying tissue were simply stripped off. It was “like peeling a banana,” said Dr. Lavallee. (The official medical term for the injury is “degloving.”)
 |
| Degloving injury to the lower leg (from Ben Ward) |
There was a white pickup truck and two men who looked official (but probably were not, thought Mark since no government employees worked on Sundays). Brian frantically told them what had happened. They had a stretcher (and, for some unknown reason, a shovel) and would help. They took Mark to the hospital on the naval base. When the ER doctor saw the gaping wound he knew that Mark needed specialist care. He immediately sent the family to St. Johns, the provincial capital and site of the only trauma hospital, one hundred miles away.
Gangrene
At St. John’s, Mark saw a British general surgeon. By then, a portion of the torn skin flap had already died, so he was treated as a burn patient with whirlpool sessions and wrapping. But his foot soon began to “turn colors.” It went from purple, to dark purple, to black. And it started to smell. The big white-uniformed orderly who had been caring for him, carrying him to and from his daily treatments, began to sob.
Mark had developed gangrene. His right foot was dying. So, after about a week, he was evacuated back to Syracuse and the next day he was seen at the Upstate Medical Center. The orthopedic and plastic surgeons there had to decide whether to take his leg off from below the knee or above the knee, in order to save him.
 |
| View of Upstate Medical Center, Syracuse (from SUNY Upstate) |
But as Mark’s horribly injured leg was unbandaged the next day in preparation for surgery his foot was, miraculously, pink. The leg (and his life) would be saved. But the extensive damage would be very slow to heal. He couldn’t walk for three years and had to get around in a wheelchair until fourth grade.
Young Mark had faith then, and he still does. (His mother sent his story to “Guideposts” and it was published). And he feels that the early and accurate diagnosis of his genetic disorder of connective tissue, knowing what he had and what he needed to deal with, helped him adapt. This was, he said, his “introduction to medicine.”
Faulty Connective Tissue
What is “connective tissue,” you ask?
From nci.org: "Connective tissue “supports, protects, and gives structure to other tissues and organs in the body. (It) also stores fat, helps move nutrients and other substances between tissues and organs, and helps repair (tissue) damage.” Much of it consists of fibers of collagen, the main structural (and most abundant) protein in the body. Connective tissue is what holds us together.
And in EDS, the formation and processing, or packing, of collagen fibrils may be altered by at least 19 different mutated genes. There are 13 (or more) types of EDS. Dr. Lavallee has what is called "classical" EDS, one of the most common forms. It can be due to many specific mutations in the COL5A1 or COLA5A2 genes.
 |
| Types of connective tissue (from quizlet.com) |
An Experience at Johns Hopkins
Johns Hopkins in Baltimore was the “only place” seeing EDS patients like him, said Mark. The field of medical genetics was being single-handedly developed by the illustrious Dr. Victor McKusick at the Moore Clinic. Disorders of connective tissue were a particular interest of his. Dr. McKusick confirmed the diagnosis of EDS and told Mark's parents that he must avoid potentially dangerous activities.
One routine clinic day, Mark (probably in the sixth grade then) was enlisted (with the consent of his parents) to help teach the “next generation of doctors” (i.e., medical students). There was a child with Marfan’s syndrome (the tall one), one with brittle bones and a misshapen skull of osteogenesis imperfecta (the short one), and Mark, with Ehlers-Danlos (the one in the middle).
Young Mark waited behind the curtain for his turn. Just before he was to go out onto the stage in the auditorium he was asked to take his clothes off so the students could see all of his scars. He did as he was told and stood there completely naked in front of about “a hundred people.” They wanted to see Mark stretch his skin, to see his joint flexibility, to see his wounds. He just wanted to put on his underpants!
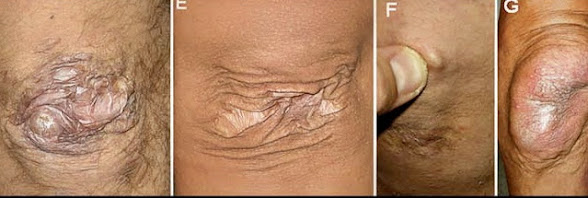 |
| Examples of skin lesions in EDS (from American Journal of Medical Genetics) |
Moving on. In secondary school, Mark was a good student, of course. But his attempts to fit in socially through athletics fell flat. He said that he “ran like Jerry Lewis” and had trouble finding his sport. It turned out that he liked wrestling and was good at it, but he was injured over and over as a result of his faulty connective tissue and poor healing. Shoulder dislocations were so frequent that he learned to fix them himself.
And as he was followed at Hopkins he had punished his scarred and deformed body (his chest wall was sunken in, a condition called pectus excavatum) so much that he was told by the experts that he was “not allowed to exercise.” He was to forego all physically strenuous activities, even gym class.
So, with an extra study hall, he had more time for books. And without afternoon sports, he had more time to eat. A typical comforting snack for the sedentary high-schooler could be two Big Macs, a large order of fries, two packs of Reese’s, and a large Coke (totaling about 2,310 calories!). His weight climbed to 230 pounds.
After high school, Mark attended Penn State as a pre-med student in the Honors program. By habit, he usually squeezed himself into the same seat in class. He said that one of his fellow students who typically sat next to him was a real “specimen.” This unusually pale classmate (looking “like Casper The Friendly Ghost’) was muscular, “he was ripped,” Mark said. They became friends and then roommates. Brett was “struggling with organic chemistry“ but Mark had “figured it out” so they made a pact; Mark would help Brett with classwork, and Brett would help Mark change his body (and his wounded psyche).
Strength Training and on to Medical SChool
Mark learned that if he was careful, and used proper technique, he could avoid injury; he could do fairly intense body-building (and strength training) relatively safely. Oddly, the gym facilities on the big campus with the well-known successful football team were limited. So Brett and Mark (with a few other investors) opened a student-run 24-hour gym. They (and anybody else at University Park) could work out whenever they wanted to. It was a huge success, such that when the young entrepreneurs later sold the gym it paid for two years of their medical school!
 |
| The huge IM Building at Penn State Main Campus: Open 9 a.m-9 p.m. (photo from PennState) |
He worked hard and he was accepted to the Hershey Medical School as a sophomore. But his father was leery about his son’s choice of career since Mark had fainted at the sight of blood (his grandmother’s, not his own) when he was home one summer during college (though it was a hot day and he had worked outside and he might have just been dehydrated, he thought).
The future Dr. Lavallee needed to test this fateful possibility. Could he practice medicine, could he be a doctor, if he had hemophobia, a morbid fear of blood?
He decided to get his license to volunteer as an EMT at State College to test this. The plan worked; he proved to himself that he could stand the sight of blood without getting sick or passing out. When he wanted to continue running with an ambulance crew over the summer break back in Maryland there was a hitch. The rule was that you had to first qualify as a level 1 firefighter. He was game, but that didn’t really turn out so well.
Let's Try Firefighting!
He went to a fire-fighting school in Maryland between his junior and senior years at Penn State. One day, there was a single-family house fire. His job was to climb the hook and ladder to get to the roof. His partner was to use a circular saw to cut holes in the roof to ventilate vertically and prevent deadly back-draft. But they were given mistaken directions; instead of ventilating away from the fire, they were directly on top of it.
The roof caved in and Mark fell through onto the floor that was in flames. His heavy breathing tank was shoved into his spine. It was hazy, black, and “extremely hot,” maybe 600-700 degrees. And he was in terrific pain. Fortunately, the experienced fire suppression team was there within seconds, but as Mark struggled to crawl to safety Army-style on his forearms and knees his protective turnout gear melted. (Continue the story...)
 |
| Efforts to produce tactical ventilation through a roof (From cfitrainer.net) |
By Anita Cherry 6/10/23


































.jpg)